Humira
With the recent approval of Humira (Adalimumab) by the FDA, there is a growing need for ulcerative colitis patient reviews of their experiences with this medication. Like some other biologics, Humira helps to stop the communication of a specific part of the immune system’s inflammatory response.
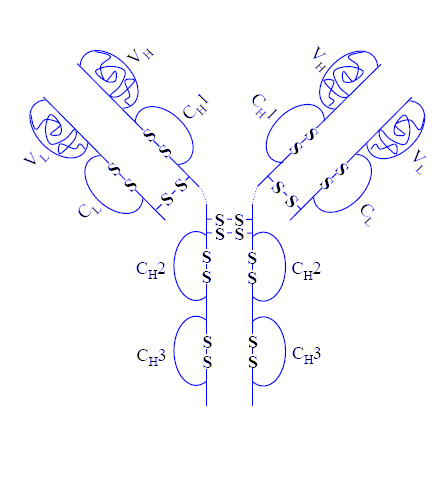
Many UC’ers are concerned that immune suppresants such as Humira will stop their immune system from working. That is not entirely true. Humira’s main goal is to stop the TNF alpha section of the immune response. (if humira stopped everything in our immune systems from working…it would be game over for everyone real quick)
Although Humira was approved by the FDA much later than Remicade which is a similar immune suppressant medication, there has been research and studies with Humira as far back as 1999 when it was still under development.
Like all medications, doctors should be consulted considerably when the decisions are being made to potentially start medications. Humira is no different. There are many reported potential side effects, and you as a patient should be well aware of what these are.
If you have experience with taking Humira for treating your ulcerative colitis, please consider leaving a review on this page of your experience.
Submit your review | |
I have hadUC since i was ten years old im now fifty. I have never been in remission for more then 8 weeks in my life and that was once. My last med before the one im on was remicade and it did not work. Im on humria and it doesnt work .just got an antibody test it was on level 3 score of 80 ,as most of you know is low. When you start humria if you dont show cliniacl improvement at eight weeks your doctor is suppose to take you off of it. Im way past eight weeks now they want to do 6mp and 40mg of humria a week, instead of every two weeks. Humria doing is 40mg every two weeks period. Sorry for the long posts ,but does anyone have some insight. Chuck
I took meslamine for 5 years and only had minor success in keeping my UC in check. After a month of Humira I am in full remission. I haven't had any side effects and have gained weight (from absorbing nutrients in my food). I will take this for the foreseeable future.
I was diagnosed 12 years ago with UC. From the start I was allergic to mesalamine, the main ingredient it meds such as Asacol, etc..
I was on prednisone for several years and went on the SCD. I was symptom free being on SCD for a couple of years and then started flaring.
in 2018, with strong recommendations from my gastro doctor, I started Humira. It basically did nothing to reduce my number of bowel movements in any way. Late in 2018 I switched to Xeljanz with no better results for 4 months. I then switch to Entyvio in May 2019. I had excellent results with my UC conditions until September when I developed a severe skin rash with hives. After a dermatologist biopsy, with was diagnosed with bullous pemphigoid which was caused by the Entyvio and have now discontinued it.
My doctor now wants me to try Stelara which was just approved by the FDA for UC at the end of October 2019. I am working to get approval from my insurance company to try it.
Bottom line is I haven't had much success with the drugs and I am running out of options. My next step is most likely surgery to have a j-pouch.
Has anyone else tried Stelara? I know it was just approved but I thought I'd ask just in case someone has some experience with it.
Thank you.
I got uc diagnosed after a trip Asia. I think I’ve picked up campylobacter and then it all started. After I couldn’t get off Cortison I was forced to take an immunosuppressive medication and most recommended it was Humira. I could get off Cortison with it. However got several infections although vaccinated of some and finally got als tuberculosis. As it’s seldom nobody thought of it. It was very hard to get the ok from the gastroenterologist to stop it. Even i was coughing very much. After 6 months of heavy tb antibiotics I got cured. 5 years I was in remission till recently. I strongly recommend not to take this drug. It’s life threatening.. also cancer is a possible side effect. I don’t believe in the 1% cancers only statistics. My doc says it’s still worth a try. He of course doesn’t have to take it.. better stay away!
I’ve been living with UC since I was 12 I’m currently 27 I’ve tried numerous medications leading up to the humira injections. For me these injections were a game changer I was in total remission was able to live such a normal life. I gave humira a 5 star rating because it was the most normal I’ve ever felt without having to take a pill every day to manage symptoms. Unfortunately I got a rare side effect from the medicine, so now I’m back to square one. I highly recommend this drug if you are looking to live a normal life.
My 18 yo son was diagnosed with UC 7 years ago, when he was 11 yo. He was started on Apriso and 6MP, which caused elevated liver enzymes so allopurinol was added to mix. He was taking 16 pills a day, including vitamins. He did great for a couple of years and then he decided that he didn't like taking all those pills every day and felt like the meds weren't working. He was about 16 and knew everything! Haha! He would miss a packet of pills here and there initially, but then just quit taking them all together after a while. He did ok for a while and felt good. Then he slowly started to decline over the next 1.5 years. He finally asked me to take him to GI because he was pretty miserable. At this point, he had lost about 35 lbs, was down to about 135lbs and 5'11". He was having about 6 watery bowel movements a day, frequent fevers up to 103° and significant joint pain. He had a repeat colonoscopy which showed moderate pancolitis. PedGI started him on Humira in Nov. of 2018. He had a good initial response after a few weeks. Most systemic symptoms, fever and joint pains, resolved and he had a slight reduction in number of bowel movements per day. Since he was 18, we just transferred from PedGI to regular GI. New GI felt that my son wasn't receiving enough Humira, so he did lab test to check Humira levels prior to his next scheduled injection. Lab test showed he had almost no Humira in his system just before his next injection. Doc is increasing his Humira to once a week, plus adding methotrexate and folic acid. We are excited, hoping he will feel better with more frequent dosing. My son has never had a single side effect from Humira and doesn't even feel the injection when I give it to him. I don't anticipate any problems with the new dosing and feel he will improve even more on new regiment.
Absolute nightmare of a drug that I wish I had not taken. Worked well for 8 months aside a constant stuffy nose and more viruses than usual . Joint pain started after 8 months, very painful , then hospitalized for a very serious opportunistic infection along with 3 types of psoriasis which has covered me from head to foot . I have a letter from my dermatologist confirming that the psoriasis is a paradoxical condition caused by Humira. The scalp psoriasis is so severe that I have lost around 60 percent of my hair and it is currently very difficult for me to walk as the soles of my feet are deeply cracked and bleed. I am a 48 year old female with no previous health conditions except for colitis. I am truly happy that this drug works for some people but I would seriously urge everybody taking Humira to be very aware of the very serious and very real side effects and to visit your doctor immediately if you experience fever, aches or rashes. The infection I had was so severe that I am lucky to be here
I used it for 18 months, went to work pretty quickly, week + and sustained pretty well but no help after about 9 months and my immune sys rejected the help.
I have been using Humira for three years. I love it. I do not get sick from colds or viruses, so i know it can compromise your immune system but i have not had that issue. It also put my psoriasis in remission.
Have been using Humira for about 1.5 years and am in full remission. I have had zero side effects. I do have to be on top of seeing the doctor as soon as I get sick but that is a small inconvenience. Very easy to manage the medication.
I started site shortly after being diagnosed in October of 2008 with severe pancolitis (when my whole colon was inflamed).
For me, it was a very rough start with severe symptoms. Getting bounced from medication to medication was not easy or too helpful. But, I did meet another UC’er, changes several parts of my diet, and of course the rest is history.
Leave a comment, ask a question, take advantage of our past experiences here, use the search boxes, they are your friends to0:)
I’ve written 2 different ulcerative colitis ebooks, you can check them out here.
And, the Free eNewsletter, which has important updates can be joined here.